Patterns of health risk factors in people waiting for elective surgery in the North East and North Cumbria


Key points
You can download a briefing paper for this work, below.
Quick-read summary
Health risk factors such as smoking, obesity, and high blood sugar are sometimes used by policy makers as eligibility criteria for surgery. For example, patients with obesity may be told to lose weight before they can have surgery.
We carried out a study to determine how many patients in the North East and North Cumbria waiting for straightforward surgeries (like hernia repairs or joint replacements) have these risk factors. We also looked at how this was spread across social groups. We used data from the Rapid Actionable Insight Driving Reform (RAIDR) database which links primary and secondary care elective waiting list data the North East and North Cumbria.
We analysed data from 78,571 patients. The most common risk factors were obesity (3 in 10 patients), high blood pressure (3 in 10 patients), high blood sugar (1 in 6 patients) and smoking (1 in 7 patients). They were significantly more common in more deprived patients. These risk factors are often used as eligibility criteria for elective surgery.
We recommend that surgical care and surgery eligibility criteria is designed and delivered with deprivation in mind, otherwise the most deprived people in society may find it difficult to access surgery and become even more unwell.
Who is this evidence useful for?
Commissioners and policy makers involved in the delivery of surgical care.
Research summary
What is the issue?
Approximately 7 million operations take place each year in the NHS. Around 60% of surgery patients need straightforward surgeries like hernia repairs or joint replacements.
Policy makers sometimes apply eligibility criteria for these surgeries. These criteria are often based on health risk factors like obesity and smoking status. For example, patients with obesity must lose weight before they can have surgery.
In a general population, people from more deprived backgrounds tend to have more health risk factors. This may make it harder for them to access the surgery they need.
People living in areas of greater socioeconomic deprivation also appear at a younger adult age on surgery waiting lists and are living with significantly more comorbidities.
We have limited knowledge on the patterns of risk factors in people waiting for surgery.
What did we do?
We analysed data of people waiting for straightforward surgeries in the North East and North Cumbria by accessing the Rapid Actionable Insight Driving Reform (RAIDR) database which links primary and secondary care elective waiting list data.
We used these data to find out how many patients were living with the following health risk factors:
We looked the odds of having these risk factors across social groups based on the England Index of Multiple Deprivation score.
What the research found
Key learning and recommendations
Further recommendations
Related information
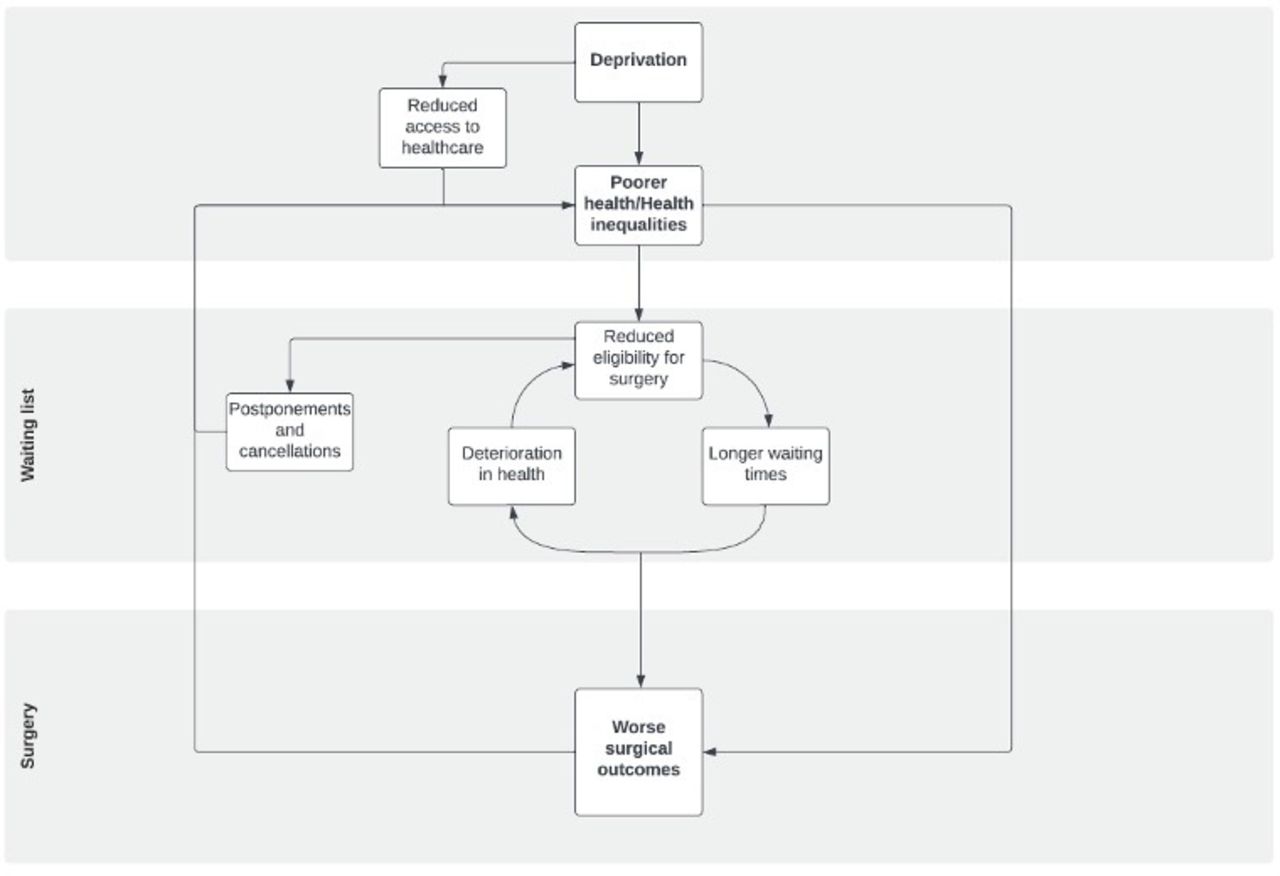
Figure: Proposed pathway showing how socioeconomic deprivation can generate and amplify inequalities in health (surgery risk factors and surgery outcomes) and care (access to surgical services) in patients needing surgery.
Download a briefing paper for this work, below.
Get in touch about this research
Dr Mackenzie Fong
Read the full research paper
Acknowledgments
This research was supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration (ARC) North East and North Cumbria (NENC) and the NIHR Leicester Biomedical Research Centre. We thank NECS for their role in providing carefully controlled access to the data, NENC Integrated Care Board (ICB) for providing the funding and leadership of the Waiting Well programme, and The Waiting Well programme board.